Abstract
Introduction The natural history of myelodysplastic syndrome (MDS) is often complicated by thrombosis and hemorrhages due to quantitative and qualitative platelet anomalies. However, there is a dearth of real-world data regarding the risk of cerebrovascular accident (CVA) in the setting of MDS. This study focuses on assessing the risk of CVA among patients with MDS in the United States.
Methods A retrospective study was performed using a large commercial US-based population database (Explorys, IBM) that aggregates records from 26 healthcare systems and includes over 80 million patients. Using Systematized Nomenclature of Medicine- Clinical Terms (SNOMED-CT), we identified adult patients (over 18 years old) diagnosed with MDS between 1999 and 2022. We examined the risk of CVA in these patients. Multivariable logistic regression was used to adjust for known variables associated with CVA such as sex, age > 65, hypertension (HTN), hyperlipidemia (HLD), diabetes mellitus (DM), tobacco use, atrial fibrillation (Afib), and the use of erythropoiesis-stimulating agents (ESA).
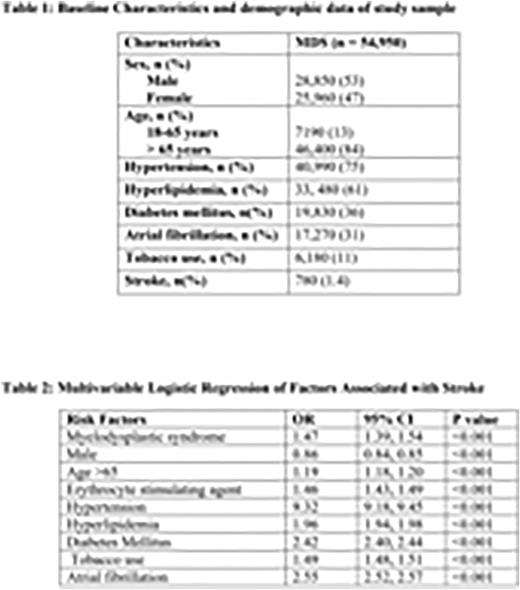
Results A total of 70,502,300 patients were included in the analysis. 54, 950 patients were diagnosed with MDS; 53% were males, 84% were above the age of 65, 75% had underlying hypertension, 61% had hyperlipidemia, 36% had diabetes mellitus, 11% were smokers, and 31% had underlying atrial fibrillation (Table 1). The incidence of CVA during the study period among patients with MDS was 1.4%. After adjusting for possible confounding factors (Table 2), MDS was independently associated with a 1.47-fold increased risk of developing CVA (OR 1.47; 95% CI 1.39-1.54; P<0.001), compared with those without MDS. The risk of CVA was also significantly higher with the use of erythropoietin stimulating agents (OR 1.46; 95% CI 1.43-1.49, P<0.001).
Conclusion This large real-world study demonstrated that MDS was an independent risk factor for CVA. With 47% higher odds, the risk is almost comparable to tobacco use. The use of erythropoiesis-stimulating agents in patients with MDS was another independent risk factor. The exact pathophysiology by which MDS increases the risk of arterial thrombosis has not yet elucidated. Further studies are needed to illustrate the possible underlying mechanisms which may lead to early interventions to decrease morbidity and mortality in this group of patients.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal